Introduction to the WHO Surgical Safety Checklist – 5 Steps
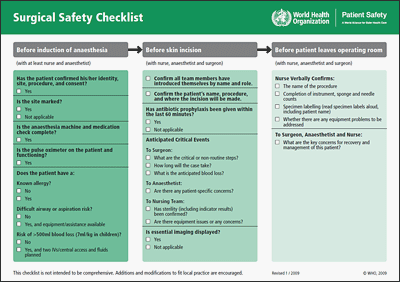
The World Health Organisation (WHO) first published their Surgical Safety Checklist in 2010. It’s a series of five critical steps that surgical teams should perform before and after surgical procedures to reduce the risk of certain adverse events.
The WHO claims that the Surgical Safety Checklist has reduced surgical complications and mortality by over 30%. Any surgical team around the world can perform the checklist in under two minutes. It’s designed to be affordable and sustainable, so that even surgical teams in low and middle income countries can adopt it.
What Are The 5 Steps to Safer Surgery?
The 2008 WHO Surgical Safety Checklist is essentially a process for improving communication between surgical teams. It involves five steps:
- Briefing
- Sign in
- Time out
- Sign out
- Debriefing
Step 1 – Briefing
The aim of the briefing is to confirm the order of the operating list, to delegate tasks and to confirm that everyone knows their role during the procedure.
The whole surgical team should receive a thorough, focused and supportive briefing before any procedure. They should feel free to ask any questions and raise any concerns they might have. Senior staff members should actively welcome queries from junior staff members.
The briefing should take place in a quiet room with a closed door, so as to ensure patient confidentiality. Any member of the team can lead the briefing, and they must encourage an atmosphere of open communication.
The briefing should begin with all members of the team introducing themselves. When discussing the patient, they should be referred to by name. Next should be an overview of the operating list – and all members of the team should have received a copy of this before the briefing. In this way, they can consider any questions or concerns in advance.
Step 2 – Sign In
The aim of the sign in is to ensure that all necessary preparations for surgery have been made, and that it’s safe to introduce anaesthesia. So all other activity must stop before the sign in, to allow the anaesthetist and Operating Department Practitioner (ODP) to give it their full attention.
The sign in process is a series of questions:
- Has the patent confirmed their identity, site, procedure and consent?
- Is the site marked?
- Is the anaesthesia machine and medication check complete?
- Does the patient have a known drug allergy?
- Does the patient have a difficult airway, or an aspiration risk?
- Is there any risk of blood loss?
These questions should be read aloud, and where necessary, the patient should be involved in the discussion. If any item in the list needs clarifying, then it must be done immediately, and the sign in process should be repeated from the beginning.
Anaesthesia should only commence once the sign in is complete, with all discrepancies resolved.
Step 3 – Time Out
The aim of the time out is to ensure that the surgical team is undertaking the correct procedure on the correct patient, and that all the correct measures are in place to prevent harm.
As with the sign in, all activity must stop to allow the team to focus on the time out. It should begin once the patient has been safely positioned with all necessary monitoring attached.
This is another series of questions which, again, should be read aloud – from the list, and not from memory:
- Confirm that all team members are present, and that all have been introduced by name and role.
- Confirm the patient’s name, procedure, and incision site.
- Anticipate critical events for the surgeon, the anaesthetist, and the nursing team.
- Ensure that all essential imaging is displayed, including X-rays, CT scans, and MRI, to reduce the risk of wrong-site surgical marking.
Surgery should only commence once the time out process has been successfully completed.
Step 4 – Sign Out
The aim of the sign out is to ensure that the surgical procedure has been completed in its entirety and documented accordingly. This step also ensures the patient’s ongoing safety beyond the theatre.
Again, all activity must stop to allow the whole team to focus on the sign out, and the sign out must be completed before any member of the team leaves the operating theatre. The patient should also remain in the theatre until any discrepancies have been resolved.
It’s once again a case of reading a series of questions aloud from a list. A surgical nurse should begin by verbally confirming the name of the procedure, before conducting thorough instrument, sponge and needle counts.
Then comes the specimen labelling process, and the nurse should read all specimen labels aloud, including the patient’s name. They should also confirm whether there are any equipment problems to address.
Finally, the surgeon, anaesthetist and nurse should confirm the key concerns for the patient’s ongoing recovery and management.
Step 5 -Debrief
The aim of the debrief is to allow the surgical team to review their performance, to identify achievements along with any areas that may need improvement.
Like the initial briefing, the debriefing should be attended by everyone. The atmosphere should be professional yet open, welcoming, and supportive.
If any actions are identified, there should be a clearly identified person appointed to deal with it. This way, everyone will know their responsibilities, which will make it much more likely that any problems will be addressed.
More Resources for Safer Surgeries
You can download a copy of the Surgical Safety Checklist from the WHO’s website. The WHO’s site also has a number of instructional videos outlining how to use the checklist, and how not to use it.
We also have a guide to standard infection control precautions in healthcare settings, and a guide to cleaning for infection prevention and control in operating theatres.
Finally, head here to read our guide to selecting the correct surgical instrument for procedures.
Want to talk about how we can help you ensure operational effectiveness in the theatre? Get in touch to talk to one of our experts today.