The Green Operating Room – Managing Spills
When it comes green operating room considerations for our NHS and private hospital customers, we focus on supplying products that are made with the environment in mind.
Not only does this help hospitals and Trusts in their own move towards Net Zero, it also helps ensure vertical integration of environmental responsibility from manufacturer through to supplier and end user.
In this article, we look at how the manufacture, distribution and design of our absorbent theatre mats pays consideration to minimal carbon emissions and unnecessary waste at all stages.
Absorbent theatre mats
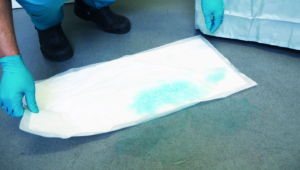
Playing an important role in fluid collection and management within the operating theatre environment, scrub areas and procedure rooms, our range of superabsorbent and anti-skid mats are high-tech products that aim for low level impact on the environment.
- Manufacturing
Our absorbent mats are manufactured using 100% renewable energy, giving an environmental impact of 0.0 g carbon dioxide (g/kWh).
The raw materials for the mats are sourced locally, minimising the number of miles travelled by component suppliers.
The mats are then manufactured using cellulose raw material from forests certified by the Forest Stewardship Council (FSC). The FSC is a non-profit organization that provides solutions to help safeguard the world’s forests and tackle deforestation, climate, and biodiversity challenges.
A focus on waste reduction during the manufacturing process also saw a 30% reduction in combustible waste during an 8-month period.
- Distribution
Once made and ready to be shipped from Europe to our warehouse in the UK, loads are optimised to ensure that as many mats as possible are shipped in one load.
As the mats are thin and lightweight and do not contain unnecessary cellulose fluff material, a large number of individual mats can be shipped in the same vehicle.
When it comes to storing and shipping mats onto our customers, we also see keeping carbon emissions to a minimum as an important goal.
As our Carbon Reduction Plan for 2024 shows, we managed to bring our Scope 1 emissions down to zero through carbon offsetting. We achieved this by investing in the Carbon FootprintTM UK Tree Planting Scheme.
As we wanted to support a local initiative, our funding will help support the planting of trees in the Yorkshire and Humber region in school locations, educate children and support local wildlife habitats.
Other measures we take to minimise carbon emissions include combining shipments to the same customer at the same time, wherever practicable; using a hybrid working model that reduces staff travel to the office; and changing much of our company car fleet to hybrid of fully electric vehicles.
- Usage
There is no doubt that the onus is increasingly on hospitals to reduce the amount of waste in operating theatres and hospital departments.
As a result, our superabsorbent floor mats are ideal for minimising waste, with one T-Mat absorbing the equivalent fluid of 13 standard inco sheets.
Our DryMax XL anti-skid floor mats also help to minimise waste, as they can be cut to the exact size required. Available as individual mats or on a 50-metre roll and dispenser, this means that you only need to use exactly the amount of mat you need on each occasion.
Interested in a mat trial for your green operating room?
We offer a range of superabsorbent and anti-skid floor mats, as well as sterile mats for use against the patient’s skin, and hybrid mats for specific procedures such as arthroscopies.
To see the whole range of our mats for your green operating room click here.
If you like what you see, then please call us on 0333 015 4345 or email info@cairntechnology.com to request samples.


