The Green Surgery Report – Surgical Products
The Green Surgery Report (a) presents the first detailed account of how to reduce the environmental impact of surgical care.
One of its focus areas is surgical products and, in particular, how to minimise waste material and energy at all stages of a product’s life cycle.
By applying circular economy concepts to healthcare products, significant carbon emission reductions can be achieved. Ways to do this include reducing, reusing, recycling, and renewing surgical products (through repair or remanufacture).
The report gives seven recommendations for making these improvements. Below we have outlined how the Stille instruments that we supply to hospitals meet these aims.
Seven Surgical Care Product Section Recommendations:
1. Ensure that design and manufacture of products minimise the environmental impact throughout the product lifespan
Stille strives to make products that can be used for decades. This reduces the consumption of raw materials as well as the energy and carbon dioxide emissions that are the inevitable by-product of prospecting, mining, enrichment, processing and transport.
By manufacturing high-quality products with a long lifespan, Stille minimizes the amount of carbon dioxide emissions per procedure for each instrument.
Some of Stille’s XE instruments are also made with more environmentally friendly Chrome-free coating. This thin layer diamond-like-carbon proprietary technology aims to reduce discoloration, improve instrument durability and help to create a more sustainable environment.
2. Ensure that modes of distribution with lowest environmental impact are chosen
By choosing to distribute surgical instruments made in Sweden, rather than further afield, such as China or Pakistan, there are fewer miles involved in shipping the instruments to our Sheffield HQ, than with some UK instrument distributors.
What’s more, as part of Cairn Technology’s yearly Carbon Reduction Plan, we constantly monitor our carbon equivalent emissions for Scope 3 Category 4, with a view to minimising these wherever possible. For example, we encourage Stille to ship instruments from several orders to us at the same time, where this is practicable for our customers.
3. Reduce and rationalise equipment
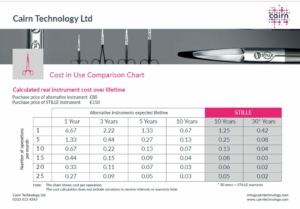
Stille surgical instruments are warrantied for 30-year of use, meaning that you can reduce the number of times you need to reorder specific types of instruments for your sets.
This in turn means that fewer carbon emissions are generated by Stille instrument usage compared to disposable instrument alternatives or reusable instruments that are only warrantied for a couple of years.
4. Switch from single-use to reusable equivalents where available
The Report says that average reductions in carbon footprint of 38-56% are achieved through switching from single-use to reusable equipment.
By choosing Stille reusable surgical instruments over single-use disposable alternatives you can not only reduce cost in use per procedure, but also the carbon footprint of your instrument inventory.
5. Optimise reprocessing of reusable equipment
Stille instruments are designed to optimise cleaning and sterilisation. Not only does the instrument coating help to reduce the risk of corrosion and pitting, the actual design of the instruments allows them to be disassembled in cases where the SSD team need access to hard-to-reach areas.
6. Extend the lifespan of reusable products through repair and remanufacturing
Stille instruments are handmade through 70 steps to optimise strength, durability and precision. What’s more, they are designed with maintenance in mind to maximize longevity.
One example of this, is the SuperCut scissors that come with a removable screw. Not only does this allow for better cleaning, but also for the blades to be restored to their original condition by Stille’s service technicians.
7. Optimise waste
By choosing Stille instruments, that in some cases have still been found in use 50 years after manufacture, you can minimise the amount of waste generated in the whole process of making and disposing of the instruments.
More tips from The Green Surgery Report
Click here to read The Green Surgery Report in full and find out other ways in which you can minimise the environmental impact of surgical care in your hospital.
To find out more about Stille instruments click here or email info@cairntechnology.com to request further information or pricing.